Appendix XV J. Cell Substrates for the Production of Vaccines for Human Use
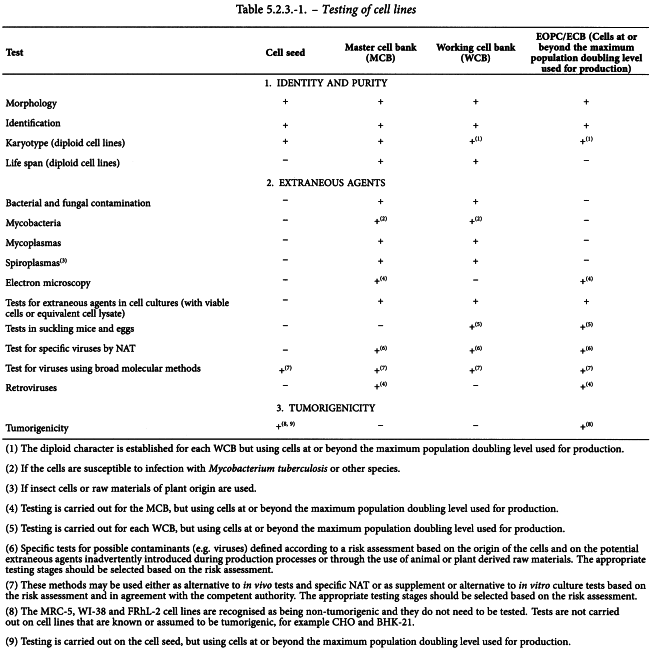
This general chapter deals with diploid cell lines and continuous cell lines used as cell substrates for the production of vaccines for human use; additional issues specifically related to vaccines prepared by recombinant DNA technology are covered by the monograph Products of recombinant DNA technology (0784). The testing to be carried out at the various stages (cell seed, master cell bank (MCB), working cell bank (WCB), end of productions cells (EOPC) or extended cell bank (ECB) corresponding to cells at or beyond the maximum population doubling level used for production) is indicated in Table 5.2.3.-1. General provisions for the use of cell lines and test methods are given below. Where primary cells or cells that have undergone a few passages without constitution of a cell bank are used for vaccine production, requirements are given in the individual monograph for the vaccine concerned.
Diploid cell lines
A diploid cell line has a high but finite capacity for multiplication in vitro.
Continuous cell lines
A continuous cell line has the capacity to multiply indefinitely in vitro; the cells often have differences in karyotype compared to the original cells; they may be obtained from healthy or tumour tissue either from mammals or from insects.
There are perceived theoretical risks associated with the use of continuous cell lines, especially if their tumorigenic potential has been demonstrated experimentally. These risks are linked to the potential biological activity of the residual host-cell DNA present in the vaccine. The residual host-cell DNA may be associated with an infectivity risk if the genome of a DNA virus or a provirus is present in the cellular DNA (either integrated or extra chromosomal). In addition, there is a potential risk of oncogenicity if the cell substrate is tumorigenic.
For vaccines produced in continuous cell lines, whether tumorigenic or not, risk assessment and risk mitigation must be performed to evaluate the suitability of the cell substrate, to define the acceptable criteria for residual host-cell DNA in the final product and to evaluate the consistency of host-cell proteins.
Cell-bank system
Production of vaccines in diploid or continuous cell lines is based on a cell-bank system. The in vitro age of the cells is counted from the MCB. Each WCB is prepared from one or more containers of the MCB. The use, identity and inventory control of the containers is carefully documented.
Media and substances of human or animal origin
The composition of media used for isolation and all subsequent culture is recorded in detail, and if substances of human or animal origin are used they must be free from extraneous agents (2.6.16) and must comply with general chapter 5.1.7. Viral safety.
If human albumin is used, it complies with the monograph Human albumin solution (0255).
If bovine serum is used, it complies with the monograph Bovine serum (2262).
Unless of recombinant origin, trypsin used for the preparation of cell cultures is tested by suitable methods and shown to be sterile and free from mycoplasmas and viruses.
Cell seed
The data used to assess the suitability of the cell seed comprises information, where available, on source, history and characterisation.
Source of the cell seed For human cell lines, the following information concerning the donor is recorded: ethnic and geographical origin; age; sex; general physiological condition; tissue or organ used; results of any tests for pathogens.
For animal cell lines, the following information concerning the source of the cells is recorded: species; strain; breeding conditions; geographical origin; age; sex; general physiological condition; tissue or organ used; results of any tests for pathogens.
Cells of neural origin, such as neuroblastoma and P12 cell lines are not used for vaccine production since they may contain substances that concentrate agents of spongiform encephalopathies.
History of the cell seed The following information is recorded: the method used to isolate the cell seed; culture methods; any other procedures used to establish the MCB, notably any that might expose the cells to extraneous agents.
Full information may not be available on the media ingredients used in the past for cultivation of cells, for example on the source of substances of animal origin; where justified and authorised, cell banks already established using such media may be used for vaccine production.
Characterisation of the cell seed The following properties are investigated:
(1) the identity of the cells, using methods such as isoenzyme analysis, in vitro immunochemical assays, nucleic acid fingerprinting and nucleic acid amplification techniques (NAT);
(2) the growth characteristics of the cells and their morphological properties (optical and electron microscopy);
(3) for diploid cell lines, karyotype;
(4) for diploid cell lines, the in vitro life span in terms of population doubling level.
Cell substrate stability
Suitable viability of the cell line in the intended storage conditions must be demonstrated. For a given product to be prepared in the cell line, it is necessary to demonstrate that consistent production can be obtained with cells at passage and/or population doubling levels at the beginning and end of the intended period of use.
Infectious extraneous agents
For cell lines for vaccine production, the testing for infectious extraneous agents must be carried out based on a risk assessment. The origin of the cell substrate as well as the potential extraneous agents that may be inadvertently introduced during production processes or through the use of animal or plant derived raw materials must be taken into account in the choice of suitable permissive cells. One such strategy is given in Table 5.2.3.-1, but alternative strategies could focus on more extensive testing at the MCB or WCB level. In any case, any strategy must be justified and lead to the same level of safety as outlined in Table 5.2.3-1. New, sensitive molecular techniques with broad detection capabilities are available, including massive parallel sequencing (MPS) methods, degenerate polymerase chain reaction (PCR) for whole virus families or random-priming methods (associated or not with sequencing), hybridisation to oligonucleotide arrays and mass spectrometry. These methods may be used either as an alternative to in vivo or specific NAT tests or as a supplement/alternative to in vitro culture tests, in agreement with the competent authority. The capacity of the process to remove/inactivate specific viruses must take into account the origin and culture history of the cell line and adventitious viruses that are known to persistently infect the species of origin, for example, simian virus 40 in rhesus monkeys, Flock house virus in insect cells or viruses that may inadvertently be introduced during production processes or through the use of raw materials of animal or plant origin. For cell lines of insect origin, tests for specific viruses relevant to the species of origin of the insect cells and for arboviruses (arthropod-borne viruses) are carried out. The panel of viruses tested is chosen according to the current state of scientific knowledge. For cell lines shown to express endogenous retroviral particles (e.g. rodent cells), the test for reverse transcriptase is not needed because it is expected to be positive, and thus infectivity tests must be performed to determine whether these endogenous retroviral particles are infectious or not.
Cell lines that show the presence of infectious retroviruses are not acceptable for production of vaccines, unless otherwise justified and authorised.
Tumorigenicity
Tumorigenicity is defined as the potential of a given cell line to induce a tumour after injection of intact live cells into immunodeficient/immunosuppressed animals (usually rodents). The tumorigenicity test is carried out using cells at or beyond the maximum population doubling level that will be used for vaccine production.
The MRC-5, WI-38 and FRhL-2 cell lines are recognised as being non-tumorigenic and further testing is not necessary. Known tumorigenic cell lines (e.g. CHO) do not need to be documented further.
When a previously uncharacterised cell line is tumorigenic, an oncogenicity study must be performed using purified DNA from the cell line and/or cell line lysate to demonstrate the absence of oncogenic components. The results are used as part of the risk analysis performed to support the use of the cell line for vaccine production. The determination of the TPD50 (tumour-producing dose in 50 per cent of animals) and the capacity to form metastases are characteristic properties that must be determined as part of the risk analysis.
Despite the difficulty in demonstrating a perfect and conclusive correlation with a tumorigenic phenotype, additional in vitro characterisation tests may be performed to document other cell substrate properties, such as the ability to grow in soft agar gels, the ability to induce invasive cell growth in muscle and/or the ability of the cell substrate to induce transformation of 3T3 cells.
Residual host-cell DNA
For each particular vaccine produced on continuous cell lines, residual host-cell DNA content must be tested and an acceptable upper limit, based on a risk assessment, must be established in the final product taking into consideration:
(1) the nature of the cell substrate (non-tumorigenic, level of tumorigenicity) and its origin (human/non-human);
(2) the presence in the production process of any steps to inactivate the potential biological activity (oncogenicity, infectivity) of the residual host-cell DNA (e.g. chemical agents such as betapropiolactone and/or DNase treatment);
(3) the capacity of the process to reduce the amount and size of the contaminating residual host-cell DNA;
(4) the intended use of the vaccine (e.g. route of administration);
(5) the method used to measure the residual host-cell DNA.
In general, a purification process for parenteral vaccines is able to reduce residual host-cell DNA in final products to less than 10 ng per dose, but the acceptance limits must be approved by the competent authority.
Once validation studies (e.g. spiking studies using an adequate size distribution of DNA) have been performed and the reproducibility of the production process in reducing residual host-cell DNA to the level expected has been demonstrated, residual host-cell DNA testing may be omitted after agreement from the competent authority.
Chromosomal characterisation
Diploid cell lines shall be shown to be diploid. More extensive characterisation of a diploid cell line by karyotype analysis is required if the removal of intact cells during post-harvest processing has not been validated. Samples from 4 passage levels evenly spaced over the life span of the cell line are examined. A minimum of 200 cells in metaphase are examined for exact chromosome count and for the frequency of hyperploidy, hypoploidy, polyploidy, breaks and structural abnormalities.
The MRC-5, WI-38 and FRhL-2 cell lines are recognised as being diploid and well characterised; where they are not genetically modified, further characterisation is not necessary.
TEST METHODS FOR CELL CULTURES
Morphology
The morphology of the cells is adequately described and documented.
Identification
Nucleic acid fingerprint analysis and a relevant selection of the following are used to establish the identity of the cells:
(1) biochemical characteristics (isoenzyme analysis);
(2) immunological characteristics (histocompatibility antigens, in vitro immunochemical assays);
(3) cytogenetic markers;
(4) NAT.
Contaminating cells
The nucleic acid fingerprint analysis carried out for identification also serves to demonstrate freedom from contaminating cells.
Bacterial and fungal contamination
The MCB and each WCB comply with the test for sterility (2.6.1), carried out using, for each medium, 10 mL of supernatant from cell cultures. Carry out the test on 1 per cent of the containers, with a minimum of 2 containers.
Mycobacteria
If the cells are susceptible to infection with Mycobacterium tuberculosis or other species, the MCB and each WCB comply with the test for mycobacteria (2.6.2). NAT (2.6.21) may be used as an alternative to this culture method provided such an assay is validated and shown to be comparable to the culture method.
Mycoplasmas (2.6.7)
The MCB and each WCB comply with the test for mycoplasmas. Use one or more containers for the test.
Spiroplasmas
Spiroplasmas may be introduced into cell substrates through contamination of raw materials of plant origin or when insect cell lines are used. When appropriate, the MCB and each WCB are demonstrated to be free of spiroplasmas using a validated method approved by the competent authority. NAT methods for detection of mycoplasmas (2.6.7) may be used to detect spiroplasmas after validation and agreement from the competent authority. Use one or more containers for the test.
Electron microscopy
The MCB is examined by electron microscopy for the presence of extraneous agents. Cell lines are maintained at the temperature routinely used for production and taken at or beyond the maximum population doubling level used for production. In addition, insect cell lines are maintained at temperatures above and below those routinely used for production and may also be subjected to other treatments such as exposure to chemical stressors. For insect cell lines the maintenance temperatures and treatments used are agreed with the competent authority, along with the number of sectioned cells to be examined.
Test for extraneous agents in cell cultures
For mammalian cells, viable cells (at least 107 cells) or the equivalent cell lysate, in their culture supernatant, are either co-cultivated (for viable cells) or inoculated (for cell lysate) onto monolayer cultures of:
(1) human diploid cells;
(2) continuous simian kidney cells; and
(3) for cell substrates other than human or simian, cells of that species, from a separate batch.
For insect cell lines, cell lysates are inoculated onto monolayer cultures of other cell systems, including human, simian and, in addition, at least 1 cell line that is different from that used in production, is permissible to insect viruses and allows detection of human arboviruses (e.g. BHK-21).
The resulting co-cultivated cell culture (for viable cells) or inoculated cell cultures (for cell lysate) are observed for evidence of viruses by cytopathic effect for at least 2 weeks. If the cell line is known to be capable of supporting the growth of human or simian cytomegalovirus, the human diploid cultures are observed for at least 4 weeks. The extended 4-week cell culture of human diploid cells, for the purpose of detecting human or simian cytomegalovirus, can be replaced by the use of NAT (2.6.21). In cases where it is difficult to keep the cell cultures healthy for the additional 2 weeks, it may be necessary to introduce fresh medium or to subculture after 2 weeks onto fresh cultures in order to be able to detect viral agents. At the end of the observation period, carry out tests on the cell culture supernatants for haemagglutinating viruses, or on the viable cells for haemadsorbing viruses using guinea-pig red blood cells. If the guinea-pig red blood cells have been stored, they shall have been stored at 5 ± 3 °C for not more than 7 days. Analyse half of the cultures after incubation at 5 ± 3 °C for 30 min and the other half after incubation at 20-25 °C for 30 min. The test for haemagglutinating viruses is not valid for arboviruses.
The test is not valid unless at least 80 per cent of the cell cultures remain viable. The cell substrate complies with the test if no evidence of any extraneous agent is found.
Retroviruses
If the cell line is not known to produce retroviral particles, examine for the presence of retroviruses using:
(1) product-enhanced reverse transcriptase (PERT) assay (2.6.21) carried out for cell bank supernatants using cells at or beyond the maximum population doubling level that will be used for production;
(2) transmission electron microscopy.
If tests (1) and/or (2) give a positive result, infectivity assays are carried out on permissible human cells with a PERT assay end-point on the supernatant.
If the cell line is shown to produce retroviral particles (e.g. rodent cell lines), examine for the presence of retroviruses using:
Since the sensitivity of PERT assays is very high, interpretation of a positive signal may be equivocal and a decision on the acceptability of a cell substrate is based on all available data.
Tests in suckling mice
The test is carried out if a risk assessment indicates that it provides a risk mitigation taking into account the overall testing package applied to a given cell substrate.
Inject 107 viable cells or the equivalent cell lysate, in their culture supernatant into 2 litters of suckling mice less than 24 h old, comprising not fewer than 10 animals;
Inject at least 0.1 mL intraperitoneally and 0.01 mL intracerebrally.
Observe the suckling mice for at least 4 weeks. Investigate suckling mice that become sick or show any abnormality to establish the cause of illness. The cell substrate complies with the test if no evidence of any extraneous agent is found. The test is invalid if fewer than 80 per cent of the suckling mice in each group remain healthy and survive to the end of the observation period.
Tests in eggs (only required for avian cell substrates)
The test is carried out if a risk assessment indicates that it provides a risk mitigation taking into account the overall testing package applied to a given cell substrate. Inject an inoculum of 106 viable cells or the equivalent cell lysate, in their culture supernatant, into the allantoic cavity of ten 9- to 11-day-old SPF embryonated hens′ eggs (5.2.2) and into the yolk sac of ten 5- to 7-day-old SPF embryonated hens′ eggs. Incubate for not less than 5 days. Test the allantoic fluids for the presence of haemagglutinins using mammalian and avian red blood cells; carry out the test at 5 ± 3 °C and 20-25 °C and read the results after 30-60 min. The cell substrate complies with the test if no evidence of any extraneous agent is found. The test is invalid if fewer than 80 per cent of the embryos remain healthy and survive to the end of the observation period.
Tests for specific viruses
The list of specific viruses to be tested is defined based on a viral contamination risk assessment in accordance with the principles detailed in general chapter 5.1.7. Viral Safety, and takes into account (but is not limited to) the origin of the cells and the potential sources of viral contamination (e.g. raw material of animal or plant origin). NAT tests (2.6.21) are carried out with or without prior amplification in cells. For cell lines of rodent origin, NAT (2.6.21) or antibody production tests in mice, rats or hamsters are used to detect species-specific viruses.
Tests for viruses using broad molecular methods
In agreement with the competent authority, broad molecular methods (e.g. High Throughput Sequencing) may be used either as an alternative to in vivo tests and specific NAT or as a supplement or alternative to in vitro culture tests based on the risk assessment.
For both NAT (2.6.21) and broad molecular methods, the stage at which testing is to be conducted (e.g. MCB, WCB, EOPC/ECB) is also based on the risk assessment and depends on the steps where viral contaminants may be introduced. In case of positive results with either broad molecular methods or NAT tests, a follow-up investigation must be conducted to determine whether detected nucleic acids are due to the presence of infectious extraneous agents and/or are known to constitute a risk to human health.
Tests for tumorigenicity in vivo
The test establishes a comparison between the continuous cell line and a suitable positive control cell line as reference (for example, HeLa or Hep2 cells).
Animal systems that have been shown to be suitable for this test include:
(1) athymic mice (Nu/Nu genotype);
(2) newborn mice, rats or hamsters that have been treated with antithymocyte serum or globulin;
(3) thymectomised and irradiated mice that have been reconstituted (T–, B+) with bone marrow from healthy mice.
Whichever animal system is selected, the cell line and the positive control cells are injected into separate groups of 10 animals each. In both cases, the inoculum for each animal is 107 cells suspended in a volume of 0.2 mL, and the injection may be given by the intramuscular or the subcutaneous route. Newborn animals are treated with 0.1 mL of antithymocyte serum or globulin on days 0, 2, 7 and 14 after birth. A potent serum or globulin is one that suppresses the immune mechanisms of growing animals to the extent that the subsequent inoculum of 107 positive control cells regularly produces tumours and metastases. Severely affected animals showing evident, progressively growing tumours are euthanised before the end of the test to avoid unnecessary suffering.
At the end of the observation period all animals, including the positive control group, are euthanised and examined for gross and microscopic evidence of the proliferation of inoculated cells at the site of injection and in other organs (for example, lymph nodes, lungs, kidneys and liver).
In all test systems, the animals are observed and palpated at regular intervals for the formation of nodules at the sites of injection. Any nodules formed are measured in 2 perpendicular directions, the measurements being recorded regularly to determine whether there is progressive growth of the nodule. Animals showing nodules that begin to regress during the period of observation are euthanised before the nodules are no longer palpable, and processed for histological examination. Animals with progressively growing nodules are observed for 1-2 weeks. Among those without nodule formation, half are observed for 3 weeks and half for 12 weeks before they are euthanised and processed for histological examination. A necropsy is performed on each animal and includes examination for gross evidence of tumour formation at the site of injection and in other organs such as lymph nodes, lungs, brain, spleen, kidneys and liver. All tumour-like lesions and the site of injection are examined histologically. In addition, since some cell lines may give rise to metastases without evidence of local tumour growth, any detectable regional lymph nodes and the lungs of all animals are examined histologically.
The test is invalid if fewer than 9 of the 10 animals injected with the reference positive-control cells show progressively growing tumours.
For a new tumorigenic cell line, in order to document the level of tumorigenicity, a dose range of cell substrate (e.g. dose of cells in the range of 105, 106 and 107) is injected in different groups of 10 animals. The number of animals showing progressively growing nodules within the animal groups is monitored to calculate the TPD50.